Menopause
Learn how to better manage the symptoms of menopause, and know where to reach out for support if you need it.
Menopause in the military
Women over the age of 50 years are a growing segment of the NZDF workforce and most will go through menopause during this time. Studies have shown around 25% of women are likely to present with difficult menopausal symptoms in the workplace. For servicewomen the impact of menopause can be significant. They are often working in male dominated environments, and the opportunity to seek supportive conversations about menopause and other health issues can be more difficult.
For some women menopause can at times affect physical fitness, sleep quality, mental clarity or mood. This can prove challenging when deploying into a field or operational environment.
The NZDF is working towards breaking down the stigma and addressing the impact of menopause from a health and social perspective while providing the support and resources women need.
What is menopause?
Menopause simply means the end of a women's menstrual periods. A normal part of ageing, usually termed after 12 months absence from menstruation. The usual age is 45-55 years.
While some women sail through menopause, some may struggle with symptoms caused by the fluctuating oestrogen and the gradual decline of progesterone.
What is perimenopause?
Where menopause is a point in time (12 months after the last period), perimenopause is the transitional state leading up to it.
When we are perimenopausal, ovulation declines while oestrogen goes up and down like a roller coaster. The follicular cycle can extend, sustaining the time oestrogen is elevated and our menstrual cycles tend to be erratic in duration and flow.
In addition, some women experience joint pain, brain fog, hot flushes, sugar cravings, irritability, increased midriff fat, night sweats and insomnia. The average woman has symptoms for 2-5 years, but up to 20% can have symptoms continue for the rest of their lives.
It’s important to note that the transition to menopause is a gradual process if it happens naturally. However, if menopause occurs as a consequence of reproductive surgery like hysterectomy (removal of the uterus), or oophorectomy (removal of one or both ovaries), menopause becomes a quicker process.
Women who smoke or have Type 1 or Type 2 diabetes may have an earlier transition and experience symptoms due to potential glucose damage of the ovaries, ovarian ageing, and other metabolic issues.
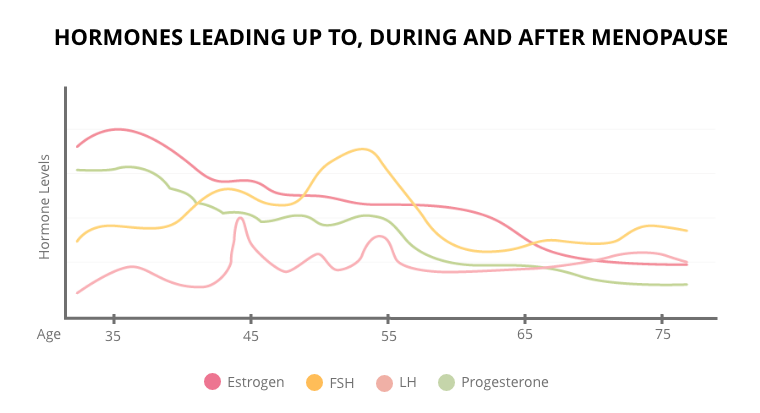
Image source. Precision Nutrition.
Menopausal weight gain
Menopausal weight gain can be a result of four related changes:
- Adipose (fat) tissue can produce small amounts of oestrogen metabolites through the aromatase enzyme, converting our androgen hormones into the oestrogen metabolites.
- We become more insulin-resistant as oestrogen declines, as it is insulin sensitising. Even with the same great diet and exercise regime we naturally are less able to tolerate the same carbohydrate load of our 20's and 30's.
- In our 40's and 50's, there is generally a lot going on. We are at the peak of our careers, our family life is full-on, often with the additional care of older parents. We can struggle too with financial concerns and relationship stresses. Juggling all of this with fluctuating hormones leads to an exacerbated stress response. Rising cortisol (stress hormone) releases glucose into the bloodstream which pushes fatty acids into the adipose (fat tissue).
- The change in relative hormone balance (decline in oestrogen) results in a relative increase in androgens, thus fat storage patterning changes, with more fat stored in the midsection.
It is the highs and lows of oestrogen before menopause that can create many of the symptoms described, rather than a gradual decline in hormones.
Common symptoms:
- Heavier periods or longer flow periods.
- Shorter menstrual cycles (less than 25 days).
- Sore, swollen or lumpy breasts.
- Mid-sleep waking.
- Increased menstrual cramps.
- Onset night sweats (particularly premenstrual).
- Migraine particularly premenstrual.
- New or increased mood swings, particularly premenstrual.
- Weight gain without changes in exercise or eating.
- Heart palpitations.
- Increased allergic reaction because of high oestrogen/low progesterone worsening histamine intolerance.
Coping strategies
What strategies do we need to put in place to mitigate some of these symptoms? If we focus our attention on the following three areas: 1) supporting progesterone, 2) metabolising and removing oestrogen and 3) reducing inflammation, we can help smooth the transition into menopause. Strategies that work for one woman might not be ones that move the needle for someone else – everyone is different, so working with a medical practitioner and having appropriate testing is recommended.
1. Supporting progesterone
Progesterone, on the slow decline, is no longer able to buffer (reduce) the effects of the higher relative oestrogen. Therefore, supporting progesterone production can be helpful. Additionally when progesterone is metabolised, one of the substances produced positively modulate's the calming neurotransmitter GABA (signalling molecule) in the brain.
If your struggling with your progesterone levels, adopting positive lifestyle changes are often more effective than supplementation. However, if a healthier lifestyle is not effective, book an appointment with your doctor to discuss Hormone Replacement Therapy as the next possible solution.
Stress management strategies
Self-care strategies, such as yoga, journaling, time in nature, meditation, or spending time with supportive friends can be very helpful.
Magnesium is well known to reduce the effects of stress. Studies show that magnesium levels drop during the perimenopausal and menopausal years, which may also impact on thyroid function.
Taurine, n-acetyl cysteine, glycine, l-carnitine, creatine and sulfurophane are other examples of nutrients and chemicals that have been studied in their ability to upregulate (increase) our glutathione production (one of the major endogenous antioxidants) and reduce the effects of oxidative stress and anxiety in the brain (read more here). Work with a medical practitioner to assess your requirement for these.
Simple dietary and lifestyle changes
- Reducing or removing alcohol
- Eliminating dairy
- Eliminating gluten
- Reducing carbohydrates
- Increasing exercise (particularly resistance exercise)
- Addressing the sleep environment
2. Metabolising and removing oestrogen
If you have more oestrogen that is causing you problems, then it is either a metabolism or a clearance problem, or both. There are different detoxification pathways through which oestrogen is pushed into the body, which require certain dietary strategies and nutrients to ensure it is done effectively, such as:
- Healthy gut microbiomes
- Iron to support Phase 1 detoxification pathways
- Brassica vegetables that contain chemicals to support oestrogen metabolism
- Omega-3 fatty acids (from fatty fish or from a fish oil supplement)
- Zinc from animal protein
- Choline from eggs and liver
3. Reducing inflammation
The dietary strategies mentioned above will all help with dampening down inflammation and should be the first line of action when trying to tackle this. In addition, turmeric (taken in a therapeutic dose, in a form that allows for better absorption such as Theracumin). Omegas such as DHA and EPA are also recommended, and you can get these by eating oily fish such as salmon and sardines, if that's not possible fish-oil supplements can help.
It is important to note that relying on plant-based sources of omega-3 fatty acids (such as chia seeds and flaxseeds) will not be adequate to provide enough DHA and EPA, as the predominant omega-3 fatty acid in plant sources (ALA) needs to be converted into DHA and then EPA, which for most people is very low. While chia seeds and flax seeds are nutrient-dense foods, they are not a replacement for oily fish or fish oil capsules. Vegetarians or vegans should opt for an algae-based supplement for their omega-3s.
NZDF support
Defence Health Centre (DHC). Make an appointment with your DHC to speak with a GP about your menopause symptoms and viable treatment options available to you. Your GP is able to refer you to specialist provider if required.
Physical activity. Speak with your local PTI or ERI for exercise advice, and check out the opening times for your nearest gym and pool facility.
Community Centre. Your local community facilitator may be able to provide you information about support groups and classes in your area targeting mature athletes.
Social Support. NZDF have access to support providers that may assist you navigating this transition - marae, social worker, chaplain or NZDF4U.
People managers
If you're a people manager think about how you can provide a supportive workplace for any of your staff who might be experiencing this transition or have concerns regarding menopause. There are plenty of helpful guides available online (below).
Useful websites
Ellen Dolgen, Health Navigator, Menopause at work, & US Medicine DOD.
Video series on menopause - (Health Navigator NZ)
